Recent developments have given researchers real optimism that advances in treatment could be on the horizon—at last.
For Michael Tsun, the first sign of trouble came late in 2012, when the Fairfax County, Virginia, resident began feeling pain in his shoulders and around his buttocks. Soon thereafter, Tsun and his physician took aim at polymyalgia rheumatica (pmr), a pain syndrome that often hits men over 50.

Tsun, then 62, started taking prednisone and methotrexate, two drugs that usually deliver PMR relief after a bit of dosage juggling and side-effect managing. But Tsun decided after six months to stop taking them. He feared that they were causing a new problem with slurred speech. Soon thereafter, his body began making too much saliva, leading to coughing fits and drooling.
Over time, his slurring problems grew worse, and he started breaking out now and again into boisterous laughter at inappropriate moments.
Tsun felt like he had seen this symptom mix before. A pulmonologist with a practice specializing in internal medicine, he had cared for perhaps half a dozen patients over the years with amyotrophic lateral sclerosis (ALS), the degenerative and deadly neurological disorder that many people know better as Lou Gehrig’s disease, after the famous baseball star who died from it in 1941.
Tsun’s ALS patients had also exhibited muscle stiffness, twitching and slurring. He now started wondering if his problems would turn out to be early steps in a frightening journey of physical decline, with leg and arm muscles growing weaker and weaker to the point of total failure, and the muscles he needed to speak, swallow and breathe following suit in short order.
“It was a very sad illness to see,” Tsun says. As a physician, all he could do was be supportive and offer palliative care.
After making this tentative self-diagnosis, Tsun retreated into a shell of denial. He did not share his worries with his primary care doctor, nor did he seek out a specialist who might confirm his suspicions once and for all.
“I was hesitant to seek help,” he says. “I knew that the prognosis was poor.”
It was Tsun’s wife, Betty, and the couple’s grown son, Matthew, an attorney, who coaxed him out of that shell. They argued that no physician could be objective when it came to a self-diagnosis like this one, and Tsun had to concede they had a point.
But when he did go see a neurologist in the spring of 2014, it turned out that his diagnosis was on the mark. Soon after that, the pulmonologist-turned-patient arrived in Baltimore to see Nicholas Maragakis, co-medical director of the ALS Clinic at Johns Hopkins.
“I was devastated,” Tsun says.
An Ambitious Project
At the moment, there is little that ALS clinicians can offer a new patient in the way of prognostic details. ALS tends to strike people in their late 50s and early 60s. Six in 10 victims are men. Nine in 10 are white. Most patients will succumb to the disease in three to four years. Others die much more quickly. A lucky few manage to hang in there—one in 10 survives for 10 years, and one in 20 makes it to 20.
Clinicians like Maragakis are unable to predict early on which new patients will land on which survival curve. Nor can they give patients reliable warnings about which mix of symptoms is likely for which cases, or how speedy and severe any individual’s decline will most likely turn out to be.
“When patients come in here, they are in a very difficult place,” Maragakis says. “They are full of questions about what’s going to happen and what they can do about it, but for the most part, they are asking things that at this point we are unable to answer in a definitive way.”
It has been like this for nearly two centuries now. Back in 1824, the Scottish surgeon and philosopher Sir Charles Bell was the first to describe a condition whose characteristics match those of ALS. It was 1874 when the French neurologist Jean-Martin Charcot gave the disease a name and pinpointed its cause in neurological problems of a mysterious nature.
It would be wildly inaccurate, however, to say that nothing has been learned about ALS over that long stretch. In fact, the important discoveries from the last few years alone are way too voluminous to catalog here.
Here is the big frustration in ALS circles: that knowledge has not yet turned into clinical breakthroughs that make a big difference for patients. Just one drug, riluzole, is approved for ALS care, and it is of modest value, helping patients live for five or six extra months.
Is there any hope on the horizon that this state of affairs might change at last?
The short answer is yes. There is a palpable sense of hope in ALS science circles these days. And that optimism very much includes a fingers-crossed suspicion that treatment advances are just up ahead on the research horizon.
The excitement is fueled in part by important new discoveries. In recent years, scientists have pinpointed a key genetic cause of the disease and begun sorting through, to an unprecedented degree, the way that mutation plays out inside the brain’s motor neuron cells.
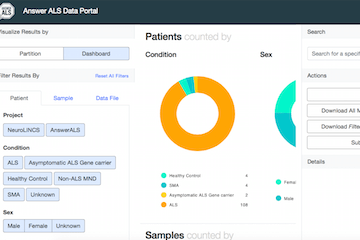
Another source of real optimism is Answer ALS, a new undertaking headquartered at the Robert Packard Center for ALS Research at Johns Hopkins. Over the next three years, that venture will build a gigantic new information repository with highly detailed data and images from 1,000 patients at five top clinics around the country.
One indication of its prospects: More than $20 million in private financing to support the project has been raised in impressively short order.
Neurologist Jeffrey Rothstein, founder and director of both the ALS Clinic and the Packard Center at Johns Hopkins, is also the architect of this initiative. To hear him describe it, Answer ALS is aiming to spark a revolution in the way scientists look at this and other neurodegenerative diseases—by bringing every scrap of new, 21st-century medical technology and scientific knowledge to bear on solving the remaining mysteries of the disease and developing treatments that really work for patients.
Not So Rare
Like many other ALS patients, Curtis Brand, 71, did not hear any alarm bells three years ago in the early days of his encounter with the disease. At first, the weakness in his knees and lower back seemed a minor annoyance. He tried a round of physical therapy. Then came surgery to straighten out a hammertoe.
Brand and his wife, Judy, started to feel genuine alarm when Curtis’ recovery from that foot surgery progressed at a snail’s pace. Soon thereafter, Brand exhibited a kind of twitching under the skin known as fasciculations.
They went to see a neurologist and then traveled to Baltimore in June 2014 to see Maragakis at the ALS Clinic. He is the one who confirmed that Brand has ALS.
Judy recalls the situation at the time of diagnosis as one of “total uncertainty” for her and Curtis. “You go online, and you try to find anything you can use,” she says. “But nothing we have done has slowed this down.”
Nonetheless, Curtis credits Maragakis with doing a remarkable job of helping him and Judy deal with their journey. Every time they leave his office, Curtis says, they do so feeling better about their situation, thanks to his warm smile and his first-rate bedside manner. They also trust that he will never serve up “false hope.”
At any given time, 30,000 people in the United States are living with ALS. About 6,000 new cases are diagnosed every year, roughly one every 90 minutes. Epidemiologically speaking, the prevalence of ALS is measured at two in 1,000, or 0.2 percent of the population. That number makes it tempting to toss around the word “rare—but that’s not a word Rothstein likes to hear.
“Is one in 500 really that uncommon?” he asks. “Don’t we all get to know at least 500 people in life? At some point, almost everyone will know a family member, a friend or, at the very least, a friend of a friend who is touched directly by this disease.”
A “Multi-omics” Approach
Answer ALS (answerals.org) aims to take the science of the disease and move it, quite quickly, into the vanguard of 21st-century medicine. There, familiar and futuristic-sounding buzzwords will come into play—personalized brain medicine, for one, along with big data and machine learning. Rothstein, the co-director of Answer ALS, ticks off a string of –omics that will be in the picture too—genomics, proteomics, metabolomics and more.
“I call it the multi-omics approach,” he says.
But the big idea behind Answer ALS isn’t all that complicated. The best clinics and labs in the land are going to gather up every single image and scrap of information those 1,000 patients have to offer. The result will be a database so chock full of detail that there are multiple hard drives of data on every individual patient.
With help from big-data experts in the private sector, Answer ALS scientists will sort through all that information in search of patterns that reveal newly discernable disease phenotypes, suggest productive lines of scientific inquiry and lead the way, at long last, to breakthroughs at the bedside.
This mix of “big data, comprehensive biological analytics, technology and science would not have been possible a decade ago,” says Clive Svendsen, director of the Regenerative Medicine Institute at Cedars-Sinai Medical Center and co-director with Rothstein of Answer ALS.
At this point, a few words of caution seem advisable. Many senior scientists in ALS circles might well experience a touch of déjà vu when it comes to all the excitement surrounding recent discoveries. Back in the heady days of the 1990s, too, it seemed like important breakthroughs were just up ahead on the research horizon.
The first time ALS was linked to a genetic mutation was in 1993. The guilty party was a gene called SOD1, which, when normal, produces an enzyme that helps the brain stay healthy over time. That enzyme is missing when the mutation is present.
This discovery sparked a flurry of research activity, including the development at Johns Hopkins of a mouse model for the SOD1 mutation. That model soon became the testing ground for lots of promising new medications, including the aforementioned riluzole, which was derived from research done in Rothstein’s lab and became, in 1995, the first ALS drug to win FDA approval.
No one would have predicted two decades would go by without a major treatment advance.
Thomas Lloyd was earning his M.D. and Ph.D. at Baylor College of Medicine in those years. He is now a Johns Hopkins neurologist who studies ALS in Drosophila melanogaster, the fruit fly.
“I can remember being in seminars where people at the front of the room were saying things like, ‘Now that we have this gene, it’s just a matter of time before we have a treatment,’” Lloyd recalls.
In the years that followed, however, scientists learned that the SOD1 mutation comes into play in just a tiny number of inherited, or familial, ALS cases. (The bulk of ALS cases are actually “sporadic,” not inherited.) In the two decades that followed the approval of riluzole in 1995, more than 100 other drugs have been tested in the SOD1 mouse model.
“Maybe two dozen of those drugs did well enough to make it into human trials,” Rothstein says. “And in the end, not one of them worked in patients. One thing I can say for sure today is that I don’t want to spend another 20 years getting results like that.”
Trio of Advances
Only time will tell if Answer ALS gets the results Rothstein and his colleagues are hoping for, but thanks to a trio of recent advances, the excitement around the project certainly seems built on more than wishful thinking.
The first of these developments came in 2007, when Japanese researcher Shinya Yamanaka showed that skin cells taken from adults could be converted back into stem cells, which can in turn be repropagated and reprogrammed into various other cell types. Yamanaka shared the 2012 Nobel Prize in Medicine for that discovery. Much of the attention paid to his advance involves hopes for regenerative medicine strategies that involve delivering healthy new cells to damaged organs.
In ALS, Yamanaka’s discovery plays out differently. Here, researchers are using induced pluripotent stem (IPS) cells as a limitless supply of motor neurons that can be studied in the laboratory as a perfect genetic match for the brain cells in any given patient.
“This is such a big change for us,” Rothstein says. In other illnesses, he notes, taking a close look at what’s happening in the cells of patients is no big deal. “But it doesn’t work that way in neurological disease. I can’t do a biopsy. I’m not going to drill a hole in the skull and draw out tissue; you can cause epilepsy that way. Patients can lose memories or become paralyzed.” IPS cell lines have given neurologists a way around that problem.
A second reason for optimism came in 2011, when two groups of researchers, one at the National Institute on Aging and the other at Mayo Clinic, simultaneously announced the discovery of a mutation in a gene called C9ORF72—C9, for short—that is involved in nearly one-half of inherited cases of ALS, along with 10 percent of sporadic cases.
That adds up to perhaps one-third of ALS cases, an unprecedented development in the field. By comparison, the SOD1 mutation discovered with such fanfare in the 1990s is involved in only about 2 percent of cases. As an added bonus: The C9 mutation is also present in one-third of frontotemporal dementia (FTD) cases. FTD is the second most common form of dementia, after Alzheimer’s.
A third piece in this fast-developing ALS puzzle surfaced in the latter part of 2015, when a team of Johns Hopkins neurologists led by Rothstein and Lloyd reported in Nature that the C9 mutation is no garden-variety affair. For one thing, the mutation lies not in the coding message, where such things usually occur, but rather in a noncoding region, called an intron, which is spliced out of the C9 gene.
“Think about a string of pearls,” Rothstein suggests. “You might assume looking at it that the shiny pearls are where all the action is, right? But the string is important too. It’s holding everything together,” and that string in this case is the intron.
To make matters more interesting, the C9 mutation does not consist, as so many mutations do, of a single isolated coding error. Where a healthy gene might have a sequence of six DNA nucleotides repeating six times in a row, that sequence is repeated “500 times, or even more” in the unhealthy gene, Lloyd says.
Picture what that does to Rothstein’s string of pearls: It’s as if the space between two pearls stretches out over a length of feet or even yards, rather than the few millimeters of gap between pearls in a healthy string.
A long-standing mystery about ALS centers on the decadeslong time lag that allows a mutation present at birth to show up as disease only after 50 or 60 years. The Nature paper includes new twists on that piece of the puzzle.
“When we put those nucleotide repeats into our fruit flies,” Lloyd says, “we saw quickly that it was causing a phenotype with that ALS-style delay to it. At birth, the neurons in those flies were normal. They only started to degenerate over time, with aging.”
To figure out why that happens, researchers in Rothstein’s lab identified more than 400 different proteins that travel along the introns. Then, in the fruit fly model, Lloyd sorted through them one by one. “If you were to try and do that in a mouse model, you might get through 10 proteins in two years,” Lloyd says. But with the fruit fly model, “we can test for hundreds of proteins in a matter of three or four weeks.”
Those tests pointed to RanGAP, a protein that normally acts as a sort of traffic cop, helping molecules move through “nuclear pores” and out into the cytoplasm of a cell. One reason the problems that arise in the C9 mutation don’t become an issue early in life is that pores become, in Lloyd’s words, “a little leaky over time.” Once that happens, RanGAP starts clumping up outside the nucleus, causing traffic tie-ups that prevent key bits of communication that it was able to facilitate back in its pre-leaky youth.
In Rothstein’s lab, researchers next looked for confirmation of Lloyd’s RanGAP clumping in brain tissue from an autopsy bank of brain tissue taken from ALS patients. They found it, fueling hope that the next research steps will lead to drugs or other therapies that can ease or bypass the clumping phenomenon and allow RanGAP to once again resume its role as the good traffic cop.
The Nature paper served up one more tantalizing, if preliminary, tidbit. In both fly cells and human stem cells, RanGAP clumping started to disappear when bits of RNA called oligonucleotides were added into cells with the C9 mutation. The oligonucleotides seemed to attach themselves to introns in ways that deactivated the problems on those elongated introns in the string of pearls.
“Between the genetic discoveries and using these cellular-based approaches to understanding the disease and developing therapies, it couldn’t be a more exciting time,” Rothstein says. The Lloyd and Rothstein labs have already set up a partnership with a pharmaceutical company interested in pursuing potential therapies, though any such development is still years away from human trials.
No Miracles
ALS clinicians often recommend that patients “lean into” the disease, preparing for its eventualities by taking proactive steps early on. It is much easier, for example, to get fitted for a wheelchair or motorized scooter before you actually need it or get used to technological options for communicating before the power of speech is altogether gone.
The Brands took this sort of approach. Late in 2014, they moved out of a stairway-filled house in Washington, D.C., and into a condo in nearby Arlington, Virginia, which they retrofitted with a number of special design features that are now coming in handy. Curtis has now lost the use of his hands, arms and legs. The Brands participated in the interview for this story over speakerphone because, while Curtis is still able to talk, it can be hard for a newcomer to make out all of his words without assistance from Judy.
In his working days, Curtis served twice as the chair of Mobil’s Saudi Arabia division. His expertise in that part of the world remains a highly valued commodity, so much so that he is serving even now on the boards of three different nonprofits in the sector: the Middle East Policy Council, American Near East Refugee Aid, and America-Mideast Educational and Training Services. He also enjoys participating in small discussion groups devoted to books and periodicals. (To read nowadays, Curtis accesses the text-to-voice function on an e-reader, then turns down the volume and reads along silently as pages turn automatically in sync with a narration that he does not hear.)
Michael Tsun, too, is learning to seek out new ways to make the most of each day. He was devastated to give up his medical practice. It was nearly as difficult to give up golf. The interviews that Tsun did for this story were conducted by email, as he can no longer speak. Unlike Brand, Tsun still has pretty good functioning in his arms and legs.
He has found his way to new hobbies—photography, travel and cooking among them. Since his diagnosis, he and his wife have been to Hong Kong and China, visiting the home villages of family members. They have also been to Vietnam, Singapore and several countries in Europe.
“I really enjoy trying to capture local people in their environs” with the camera, he says. Both the Tsuns and the Brands follow the news on the latest ALS findings coming out of neurology laboratories, but neither is obsessive about it. Like most other patients, the two have also found their ways to strategies that, while still unproven, feel right for their individual journeys. Tsun gets regular acupuncture treatments. Brand followed a ketogenic diet when he was still eating on his own; he is now on a feeding tube.
“We have a good perspective on things,” Brand says. “We know that there are no miracles around the corner for us.”
Cautiously Optimistic
As modern-day scientific endeavors go, Answer ALS has several unique qualities. It has more of a corporate aura than the standard academic endeavor, with ambitious milestones clearly laid out on a strict timetable for all to see. In addition, the humongous database that Rothstein and Svendsen are coordinating of those 1,000 patients will be an open-source affair, accessible without restriction to researchers around the world.
The private fundraising aspect of Answer ALS is important too. It will allow each of the five participating clinics to hire a full-time coordinator dedicated solely to the project. “Just in the last few years, really, people are becoming excited again,” Lloyd says. “There really is a feeling in the air that we might be getting close, not just to a new understanding of the disease, but also to figuring out what to do about it on the treatment side.”
Maragakis agrees. “I’m much more confident now that our therapeutic targets are broader than ever and that we will really be able make a dent in ALS in the coming years, and perhaps even cure it.”